Products You May Like
Using a sperm donor wasn’t part of Rachel Seltzer’s life plan. The Atlanta-based operations director always wanted to be a mom, but she spent her 20s and 30s in long-term relationships that didn’t work out. After turning 37, she was convinced it was too late—the idea of meeting a partner and having a baby in her remaining reproductive years seemed impossible—but a conversation with her therapist convinced her that she didn’t need a man to move forward. She could do it on her own.
Her story is familiar for many women, who are increasingly using sperm donors to build families, with or without partners. Perusing profiles on sperm donor websites is “like being on Match.com, but in reverse,” said Cari Rincker, who was 37 when she went through a breakup and decided she was ready to find a sperm donor to use with her frozen eggs.
Users can search for donors by education level, hair color, race, and height, all while looking at pictures of donors as babies or kids. But it’s not all fun and games. Picking a sperm donor can be an emotional process, Rincker explains, because it doesn’t necessarily line up with the fairytale that many women dream of.
And how do you know what to look for, anyway? Some women confess to being hyper focused on height, while others are dead set on finding someone with a master’s degree. But what actually matters, and how do you know when you’ve found The One? I spoke to women who went through the sperm donor selection process about how it works and what they learned along the way.
How do you start the process?
Going to a fertility clinic is the first step in the process, and while picking a doctor you’re comfortable with is important, you don’t need to worry too much when it comes to landing on a sperm bank. Most sperm banks are FDA compliant, and there isn’t really a risk involved in choosing any one of them, Dr. Zaher Merhi, medical director at Rejuvenating Fertility Center in New York City, said.
Fertility doctors will walk you through all of your options when it comes to getting pregnant, and oftentimes, they’ll even guide you in the direction of a specific sperm bank. After speaking to a fertility specialist, Seltzer signed up for an account on the California Cryobank website, one of the most popular options.
The sign-up process is simple. First, you pick a cryobank website that feels like a good fit for you. With a simple Google search, you’ll come across a wide range of options, and as Dr. Merhi said, you really can’t go wrong. It’s important to note that you don’t have to live in the area where the cryobank is based in order to qualify for receiving donor sperm. For example, you don’t have to live in California to use the California Cryobank.
Once you pick a sperm bank that feels like a good fit for you, you create an account on that website. You can pay for à la carte options as you look through the donor profiles, depending on the information you want access to. On California Cryobank, a popular sperm donor website, for example, users can look at donor profiles, medical histories, personal essays from the donors, and staff impressions of the donors for free, but additional features come at an added cost. For a bundle that includes extended profiles, childhood photos, and the “Express Yourself” feature, where donors are encouraged to describe who they are, you have to dish out $145, but doing so gives you access to the extended profiles, etc. for all the donors you search through. You can also add features to your experience. A handwriting analysis, for example, will cost you an additional $25.
Buying sperm is a lot like buying anything else you’d purchase online. “You basically add them to your cart—the way you would anything at Amazon,” said Holly Meloy, a managing partner at a design firm, who decided to pursue motherhood on her own at age 37. For most sperm bank websites – including California Cryobank and the Fairfax Cryobank, the sperm can cost anywhere from $500 to $1,300, depending on specific factors like whether or not the donor wants to be contacted.
Are all donors anonymous?
For many women, picking an anonymous donor is important. Seltzer specifically looked for a donor who chose to be anonymous, and she wanted it to be as private as possible. “A donor is someone that chooses to help others, and that’s all it is,” she said. “It’s not family,” she added. “It’s strictly to help those that need sperm donors.”
But sperm can come from both anonymous donors and open donors—those who consented to at least one form of agreed-upon communication from their offspring when they turn 18. And there isn’t necessarily a price difference; both options cost $1,045 at California Cryobank, for example. But for ID donors—those who allow the future child to request the donor’s identifying information when they turn 18—the sperm costs $1,245.
What’s the difference between IUI, IVF, and ICI?
Sperm donor material is used to conceive a baby if there isn’t viable sperm available. After the sperm is purchased on a cryobank website, it is sent to the hospital or clinic where the insemination process eventually takes place.
There are three processes you can pursue once you acquire the donor sperm: intrauterine insemination (IUI), in vitro fertilization (IVF), or intracervical insemination (ICI).
During IUI, the doctor places sperm directly into the uterus with a small catheter. This process aims to improve the chances of getting pregnant by increasing the number of healthy sperm that ultimately reach the fallopian tubes when the woman who is trying to get pregnant is most fertile.
With in vitro fertilization IVF, the patient undergoes a range of procedures. Mature eggs are collected from the woman’s ovaries and fertilized—by donor sperm, in this case—in a lab. The fertilized eggs are then transferred to the woman’s uterus. Ultimately, one full cycle of IVF can take about three weeks, and sometimes the different steps of the process are split up, which can drag things out longer.
In the ICI process, the doctor uses a syringe to place the donor sperm directly inside of the woman’s cervix.
What do you need to do before picking a donor?
Doing your homework is important, of course, and genetic testing is a big part of that. The first step is to go to your doctor and get a genetic carrier screening. The test, which is typically a blood or saliva test, checks for recessive genetic disorders like cystic fibrosis, tay-sachs, and thalassemias.
It’s also important to check your Cytomegalovirus (CMV) status, a herpes virus that becomes latent after a primary infection, but can reactivate at a later time and shed virus. Before purchasing donor sperm, a patient should make an appointment with a physician first to discuss this part of the process, said Dr. Kimberly Thronton, an OB-GYN and reproductive endocrinologist at Reproductive Medicine Associates of New York. In these cases, the physician typically routinely orders the CMV test, which is separate from the infectious disease test. “A patient could ask for this separately, but their physician should routinely order it if they know they are planning to use donor sperm,” she said. If not, as a patient, you can specifically ask for it.
If you’re CMV negative, it’s best to pick a CMV negative donor; if you’re CMV positive, you can pick either a negative or a positive donor. If you are CMV positive, you have already had a prior infection and have antibodies, Dr. Thornton pointed out. This means you are not at risk for acquiring CMV through sperm. About one in every 200 babies is born with congenital CMV, according to the CDC. Most people who have been infected don’t have symptoms, and that’s why it’s important to get tested.
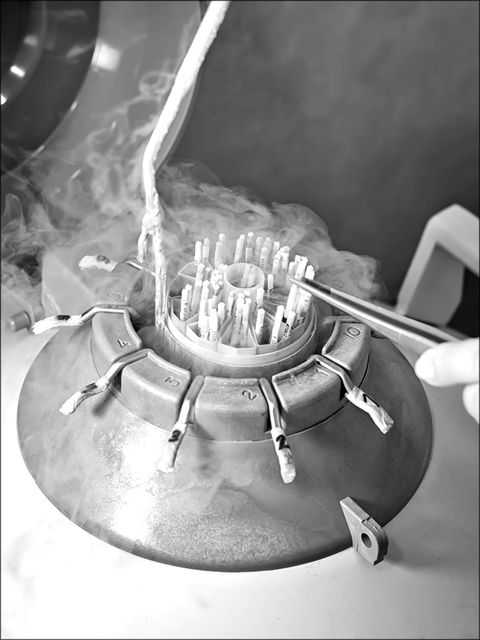
“Typically the doctor’s office will just check and verify paperwork given by the sperm bank to make sure there are no medical issues or concerns regarding the selected donor,” said Dr. Thronton. Once everything checks out, the sperm banks typically ship the sperm directly to the doctor’s office in storage tanks.
Most women have personal preferences when it comes to things like education level, hair color, eye color, race, and height, but CMV status and genetic screenings should be prioritized first and foremost, according to experts. After that, “the non-medical fun party kicks in, and they can apply those preferences,” Dr. Thornton added.
How do you know the sperm is safe?
Doctors evaluate the donor’s genetic screening and CMV results and perform vigorous infectious disease testing, testing for diseases like HIV, hepatitis B, Zika, and West Nile Virus. Donor sperm has to be frozen and quarantined for three to six months to ensure that the donor does not have infectious diseases that could be transmitted through insemination, Dr. Thornton said. This process legally protects both the donor and the intended parent.
Fertility centers will also check to make sure the sperm donor has adequate sperm on a semen analysis. This test also determines if the donor is fertile, if the woman is working with a donor she knows. If you’re purchasing from an anonymous donor, however, the sperm bank checks the donor’s fertility in advance.
How do you narrow down the list of potential donors?
Narrowing down the list of potential donors comes easy for some women, but for most, the number of options and factors to consider can be overwhelming. It’s also important to have backups. “I’ve seen women get their hearts set on a donor and they’re so into it, and then the sperm is not available, and they’re devastated,” acupuncturist and fertility expert Aimee Raupp said. “There’s this real connection that can get formed.”
One of Raupp’s clients had a child with donor sperm and wanted to use the same donor to have a second child, but the donor didn’t have any other samples available. To avoid this, you can inquire about how much sperm you would need at the outset for getting pregnant and growing your family. “Ultimately, it was a lack of education, resources, and support that led to this problem,” Raupp pointed out. Women should make sure there are multiple samples available from the same donor if they’re interested in using the same person’s sperm to have another child in the future. You can buy several samples at once and save them for future use.
Evaluating the compatibility of the donor’s stats and sample—and having more than one option—is important. Once Seltzer narrowed down her decision to two donors, she printed out all of their information and shared it with her family and a couple of close friends. She was looking for someone who was tall and athletic, with dark hair and brown eyes, but above all, she wanted a donor who was highly educated. Her family and friends looked at the profiles and gave her feedback that helped her make her final decision. Before selecting him, Seltzer got to hear an interview between the donor and one of the employees at the sperm bank. “I loved his voice,” she said, adding that he sounded like someone she would love. “It was a perfect match.”
Meloy was also very methodical about her sperm donor search and final selection, creating a detailed spreadsheet that she shared with her close friends and family. She ruled out donors who had a family history of alcoholism and focused on health history, education and head size—yes, you read that correctly—as her priorities. With this in mind, her loved ones used a carefully curated checklist to narrow down the list of sperm donors.
How did the recent SCOTUS ruling impact sperm donation?
The climate surrounding terminating pregnancies shifted dramatically this year. Dobbs v. Jackson, a landmark SCOTUS decision in which the court held that the US Constitution does not grant women the right to an abortion, has “limited the treatment options many physicians are able to offer their patients,” Dr. Thornton said. In some states, women are being forced to carry pregnancies to term only to watch their child die after birth.
“In the fertility realm, there is a lot of concern how the overturn of Roe will impact patients utilizing IVF for both infertility and fertility preservation such as egg and embryo freezing,” Dr. Thornton said. Some states have been attempting to enact personhood laws that consider every embryo a legal person. This means embryos created via IVF could be at risk. Ultimately, personhood laws have the ability to limit or ban access to IVF. They also lower success rates and drive up the costs of IVF.
Is the process stressful?
The process is definitely stressful and filled with so many decisions and factors, but the women I spoke to said every moment of stress was worth it.
For Seltzer, picking a donor was stressful and anxiety-inducing, but after she landed on her final pick, she felt excited and confident in her selection. Her son Aiden is three years old now. “He makes my days bright and my life much more fulfilled and happier,” she said, adding that she’s become more joyful and stronger after having him.
Rincker felt excited about the process at first, but ultimately, it wasn’t an easy journey. “The period of my life trying to become pregnant was an emotional roller coaster,” she said. Now she puts her son, who is almost a year-and-a-half now, to sleep every night and is reminded of the love he adds to her life. “In some ways, my family is nothing that I would have dreamed for myself,” she said. “But in other ways, I have more than I ever could have hoped for.”
Meloy also said the process was “very stressful,” and she cried after buying donor sperm for the first time. “I had suddenly made this massive decision on behalf of my unborn child,” she recalled. She remembers asking herself if she made the right choice. She wondered, “Will my future child be okay? How much of growing up is nature versus nurture?” But now, her daughter—who she gave birth to thanks to a sperm donor—is almost seven years old. “Every year on her birthday, I say a solid thank you to the man who we will never know, but who gave me the greatest gift anyone could ever give me.”
Alexis Benveniste is a writer and editor who proudly interned at ELLE many moons ago; her work has been featured in The New York Times, The Washington Post, Vanity Fair, Bloomberg, and other notable outlets.